Pelvic floor physical therapy offers relief for silent problem
Pelvic floor physical therapy is rarely talked about outside of the doctor’s office. However, this nonsurgical approach to rehabilitating dysfunctions of the pelvic floor that contribute to bladder, bowel, sexual health and pain complaints can benefit many women and men.
“These are conditions that people don’t easily talk about, especially if they think there’s no help for them,” says Dr. Jaime Long, a urogynecologist with Penn State Health Women’s Care. “The more we can educate patients about what is available, the more we can change that mindset.”
Long has always believed it was important to have a pelvic floor physical therapist on staff at Penn State Health St. Joseph, so she was pleased when Margaret Homan joined Penn State Health St. Joseph ― Strausstown in September 2019.
“Almost everyone who suffers from a pelvic floor disorder — whether urinary incontinence, prolapsed bladder, pain or other problems — will see great benefits from physical therapy,” she says. “Having someone I can connect them with and have communication with regarding joint treatment efforts is very, very useful.”
Homan has been a physical therapist for 27 years and completed training in pelvic floor therapy. While the majority of her career has been in hospital-based outpatient orthopedics, a personal experience led her to focus on pelvic floor therapy.
“I was having a pelvic floor issue myself and was referred to a pelvic floor physical therapist by my gynecologist,” she says. “Then I started my own self-help program. I decided I wanted to help other people with this very real problem.” Incontinence is just one example of pelvic floor dysfunction. Many people think it is a part of growing older, but it is also fairly common in female high school and college athletes. “The jumping, running and push to do core stabilization can cause a short, tight pelvic floor and lead to stress urinary incontinence.”
The pelvis is a network of muscles that serve as a bowl to keep the organs in place and help them function as an integrated system. When those muscles suffer from dysfunction, they can benefit from physical therapy, according to Long.
“Physical therapy works to strengthen muscles that are weak and relax muscles that might be too tight,” she says. “In cases where patients have difficulty controlling their bowels or bladder, it is such a socially devastating problem that they are often very invested in getting better.”
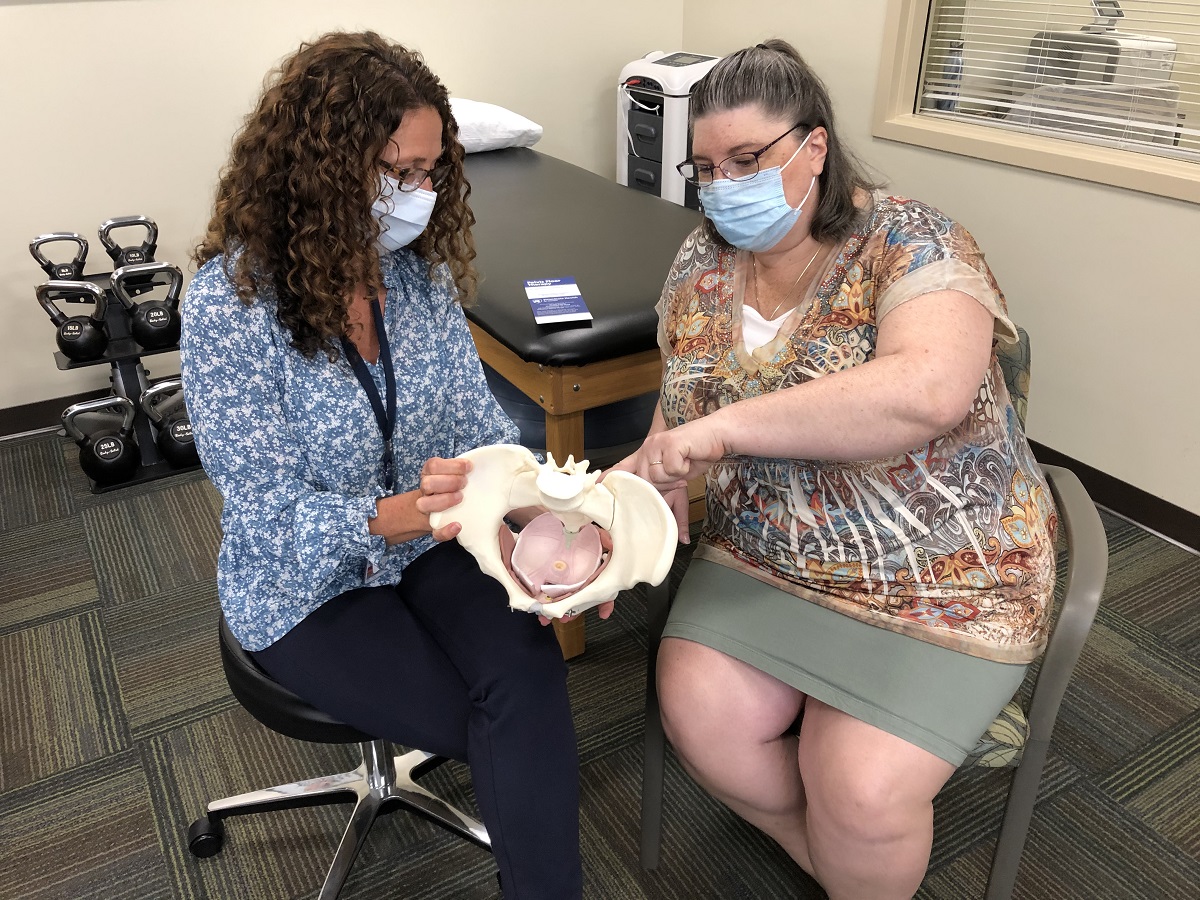
Once armed with a diagnosis, Homan uses an individualized approach with patients that may include behavioral strategies, manual therapy, biofeedback, modalities, therapeutic exercise, education and functional retraining.
“By the time a patient gets to me, they are desperate for help,” she says, acknowledging that having personal experience with pelvic floor issues makes it possible for her to better relate to her patients. “My desire is to help patients cope with a silent problem that affects many people and make it possible for them to lead a more functional life.”
If you're having trouble accessing this content, or would like it in another format, please email Penn State Health Marketing & Communications.
