Researchers design clinical trial to test use of exercise for severe liver disease
A team of Penn State researchers developed a first-of-its kind clinical trial to test the use of exercise as a treatment for patients with a severe form of nonalcoholic fatty liver disease.
Nonalcoholic fatty liver disease is the leading cause of chronic liver disease in the United States. People with this disease have an extra fat build up in their liver cells not caused by drinking alcohol. It often affects people who are overweight, obese, have diabetes or those with high cholesterol.
Nonalcoholic fatty liver disease can become a more severe condition called nonalcoholic steatohepatitis – often called NASH. NASH, with a lack of exercise, can lead to liver cancer or end-stage liver disease requiring liver transplantation. NASH is already the most common reason for liver transplantation in women and is soon expected to be the most common reason for both men and women by 2025.
Patients with end-stage liver disease from NASH have a greater risk for blood clots, including clotting in the blood vessel that brings blood to the liver from the intestines. A blood clot in this vein may prevent a liver transplant from happening and shortens survival after transplant.
Exercise can lower clotting risk in both healthy people and people with vascular disease. For this reason, researchers want to learn if a supervised aerobic exercise program reduces levels of a specific protein that leads to blood clots in patients with NASH. The researchers designed a first-of-its kind clinical research study, called NASH Fitness Intervention in Thrombosis – NASHFit – to investigate this possible treatment. The study design was recently published in the journal Contemporary Clinical Trials Communications.
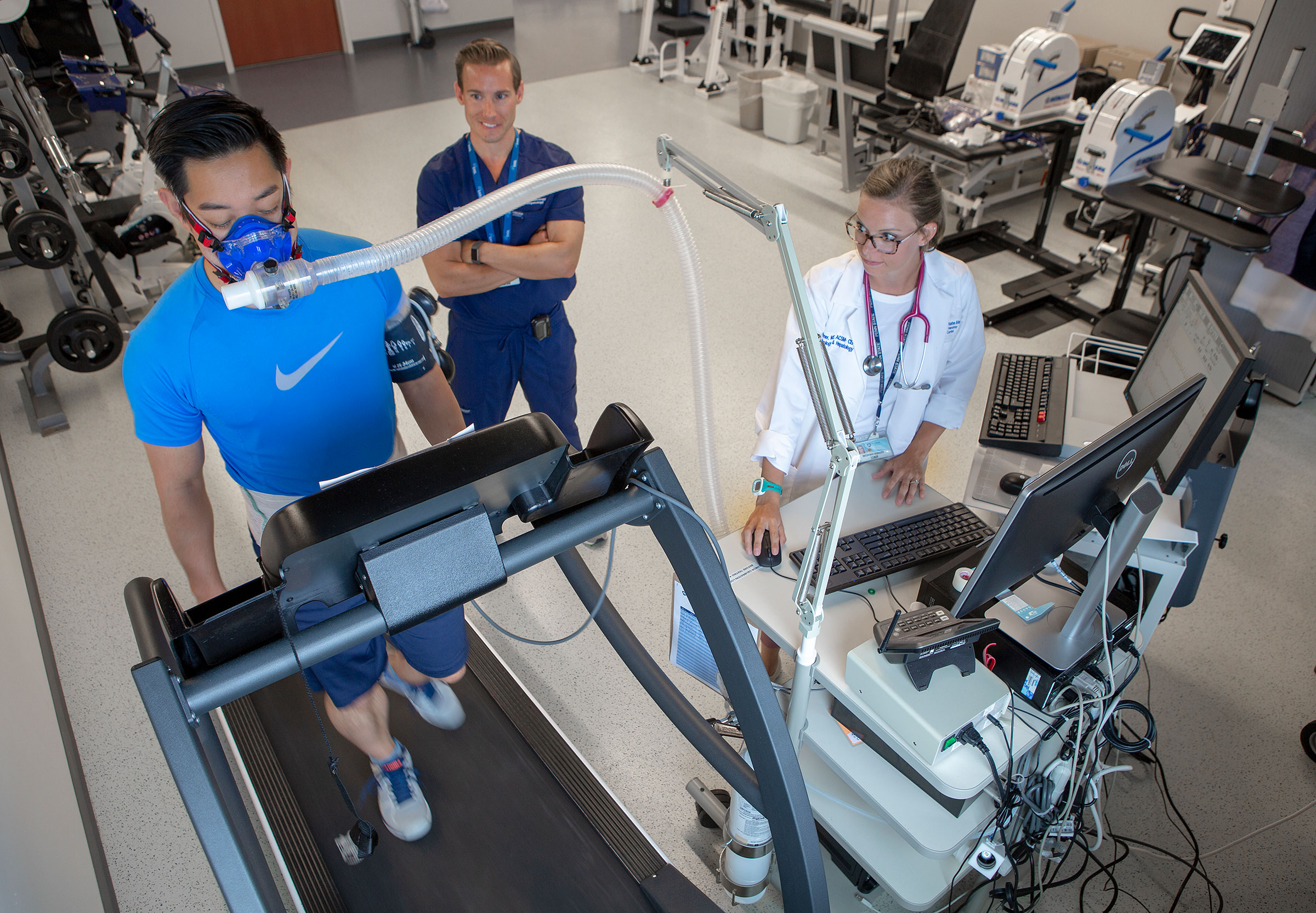
Researchers will study patients who will be randomly assigned to one of two groups. One group will receive 16 weeks of exercise training which includes supervised aerobic exercise sessions with an American College of Sports Medicine-certified exercise physiologist and dietary counseling from a registered dietician. The control group will be asked to maintain their current clinical care at the direction of their health care provider. Members of this group will receive basic information from the American Liver Foundation to reinforce the guidance of the healthcare provider. The participants will receive weekly phone calls from the study team.
Researchers believe that the specific blood clot creating protein will be significantly reduced in participants who receive the exercise training. The study will determine if their belief – called a hypothesis – is accurate. Other related measurements that will be collected include levels of liver fat, liver scar tissue, physical fitness, body fat composition, weight and quality of life.
The study of the use of exercise in patients with NASH is important because drug treatments are often ineffective and have significant side effects.
“The timing of the NASHFit study is crucial given the worsening epidemic of metabolic disease,” the researchers wrote in their paper. “As most NASH patients are asymptomatic and our diagnostic testing is ineffective in discerning which persons will have disease progression, this combination is the perfect milieu for progression to end-stage liver disease which may require lifesaving liver transplantation.”
Researchers will recruit 42 participants for the study. NASHFit will use Clinical Research Center, a resource of Penn State Clinical and Translational Science Institute, for some study visits. Clinical Research Center provides research infrastructure including specialized nursing support and administrative services for human subjects research. These dedicated research units are located at Penn State Health Milton S. Hershey Medical Center in Hershey and Noll Laboratory at Penn State University Park.
“We are very fortunate at Penn State Health and Penn State College of Medicine to have access to the immense research resources of both Clinical Research Center and Penn State Clinical and Translational Science Institute,” Dr. Jonathan Stine, Penn State Health Liver Center research director and principal investigator, said, adding that without this infrastructure, the leading-edge science being performed in the NASHFit trial would not be possible, and patients would not have access to the important exercise training they need to improve their fatty liver disease. Learn more about Stine’s research here.
The study team includes Stine, Dr. Ian Schreibman, Seyedehsan Navabi, Mitchell Kang, Jessica Dahmus, Gloriany Rivas, Breianna Hummer, Megan Byer, Heather Tressler, all of Division of Gastroenterology and Hepatology, Department of Medicine; Christopher Soriano and Dr. Christopher Sciamanna, Department of Medicine; Scot R. Kimball, PhD, Department of Physiology; Andrew D. Patterson, Department of Biochemistry and Molecular Biology and Kathryn Schmitz, PhD, Departments of Kinesiology and Physical Medicine and Rehabilitation. Stine, Sciamanna and Schmitz are also with the Department of Public Health Sciences and members of Penn State Cancer Institute. Stine and Schreibman are with Penn State Health Liver Center.
National Institutes of Health (L30 DK118601), Pennsylvania Department of Health using Tobacco CURE Fund, and National Center for Advancing Translational Sciences through Penn State Clinical and Translational Science Institute (UL1TR002014) funded this project.
If you're having trouble accessing this content, or would like it in another format, please email Penn State Health Marketing & Communications.
