The Medical Minute: Is it a sports injury or growing pains?

There was nothing overly dramatic about Madelyn Olympia’s injury – unless you’re a 14-year-old volleyball player. While she didn’t suffer an epic tear or collapse on the court, a few months ago, she started experiencing back pain after diving for a ball.
“The first time it happened, I was just diving normally, but something sounded different,” Olympia, of Hummelstown, says. “After that, it hurt every time I bent forward and back.”
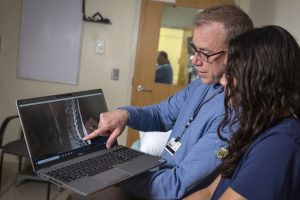
Madelyn’s parents knew that back pain at age 14 wasn’t normal, so they scheduled an appointment with Dr. Matthew Silvis, a sports medicine physician at Penn State Bone and Joint Institute and professor of orthopaedics and rehabilitation at Penn State College of Medicine. As team physician for the Hershey Bears ice hockey team and Hershey High School teams, Silvis looks for more than just traumatic sports injuries. He also keeps an eye out for a common but often overlooked issue in student athletes: repetitive use injuries.
An MRI confirmed his suspicions for Madelyn – she had strained her back muscles. His prescription? Rest and physical therapy.
Know the signs of overuse
Traumatic sports injuries – like broken collarbones, torn ligaments and concussions – sideline countless student and professional athletes. But acute injuries are only one side of what Silvis sees on a regular basis.
“Overuse injuries are really predictable,” Silvis says. “We use the ’rule of toos’ – too much, too fast, too often. When kids are in the position to overuse certain muscle groups or joints, that’s when they start to break down and have injuries.”
Silvis says that he seldom sees student-athletes at the time of their injury. Instead, they’ve typically experienced soreness or aching for weeks or months, which then develops into enough pain to indicate an injury. He says that many parents and coaches mistakenly attribute this pain to normal ‘growing pains,’ but Silvis warns that dismissing these concerns can lead to more serious injuries.
“It’s likely not a growing pain. It’s the onset of an overuse injury, and when that happens, eventually the student athlete can’t participate in their given sport,” Silvis says.
One way parents and coaches can identify injuries is to know what to look for. Signs of injury can include:
- Swelling of joints or soft tissue
- Tenderness in a specific point of the body
- Missing practices due to pain
Listen and act early
One of the best ways parents can help their kids stay in the game is to listen to their concerns and act early, says Silvis. With swift attention to pain and discomfort, he says student-athletes can often continue to play while healing, while ignoring pain for too long may mean they have to take a break from sports completely to heal.
“Anchoring coaches and parents to sport guidelines can really help. Take baseball, for example. If we follow USA Baseball’s recommendations for pitch counts, we can avoid overuse injuries to the shoulder or elbow,” he says. “We might recommend runners decrease the number of miles they run by 50% until their overuse injury starts to heal, and they no longer have discomfort. But that way, they still get to participate, and they can be social with their friend group.”
Avoid same sport stress
Madelyn, like many student-athletes, pushes herself to excel, and what was once an annual season for volleyball has now become a year-round pursuit. Pediatric specialization, or letting a child under age 12 focus on one sport for more than eight months a year, can lead to overuse injuries. Fortunately, Silvis says there’s an easy way to avoid those injuries – parents can encourage their kids to diversify their activities to work their bodies in different ways.
Silvis co-authored a 2018 study on pediatric sports specialization in elite ice hockey players. His research found that top-level players usually started specializing
in that sport at age 14. Early specialization didn’t increase their odds of excelling and can increase risk of overuse injuries.
That doesn’t mean that students have to sit out a season altogether. The key is to use different parts of the body throughout the year.
“It’s not a problem if the sports are different. If you golf in the fall, play basketball in the winter and run track in the spring, you’re using different parts of your anatomy,” Silvis says. “It’s a much bigger problem if you’re playing the same sport year-round. So the diversity in the balance of activities is really the key.”
Back on track
With a diagnosis in hand, Madelyn began physical therapy to strengthen her core and support her back.
“At physical therapy, I focus on exercises that strengthen my core so the muscles around it are stronger,” Olympia says. “Each time, the physical therapist makes the exercises a little bit harder so I can work back up to where I want to be.”
Outside of physical therapy, Silvis encourages Madelyn to play more mindfully.
“I’ve been able to work with her on some volleyball boundary setting in terms of how often she’s diving for balls, et cetera,” Silvis says. “After her season is over, she’s promised me she’ll take a break for a season of rest.”
Related content:
- The Medical Minute: Return to play after injury — What athletes and families should know
- The Medical Minute: Aerobic exercise speeds recovery for adolescents with sports-related concussions
- Video: When should you seek medical help for a concussion? Penn State Health Sports Medicine
Find a Penn State Health sports medicine doctor near you.
Learn about sports medicine clinical trials at Penn State College of Medicine.
The Medical Minute is a weekly health news feature produced by Penn State Health. Articles feature the expertise of faculty, physicians and staff, and are designed to offer timely, relevant health information of interest to a broad audience.
If you're having trouble accessing this content, or would like it in another format, please email Penn State Health Marketing & Communications.