The doctor will ‘see’ you now, virtually: Telehealth program saves patients miles, time and energy
By Carolyn Kimmel
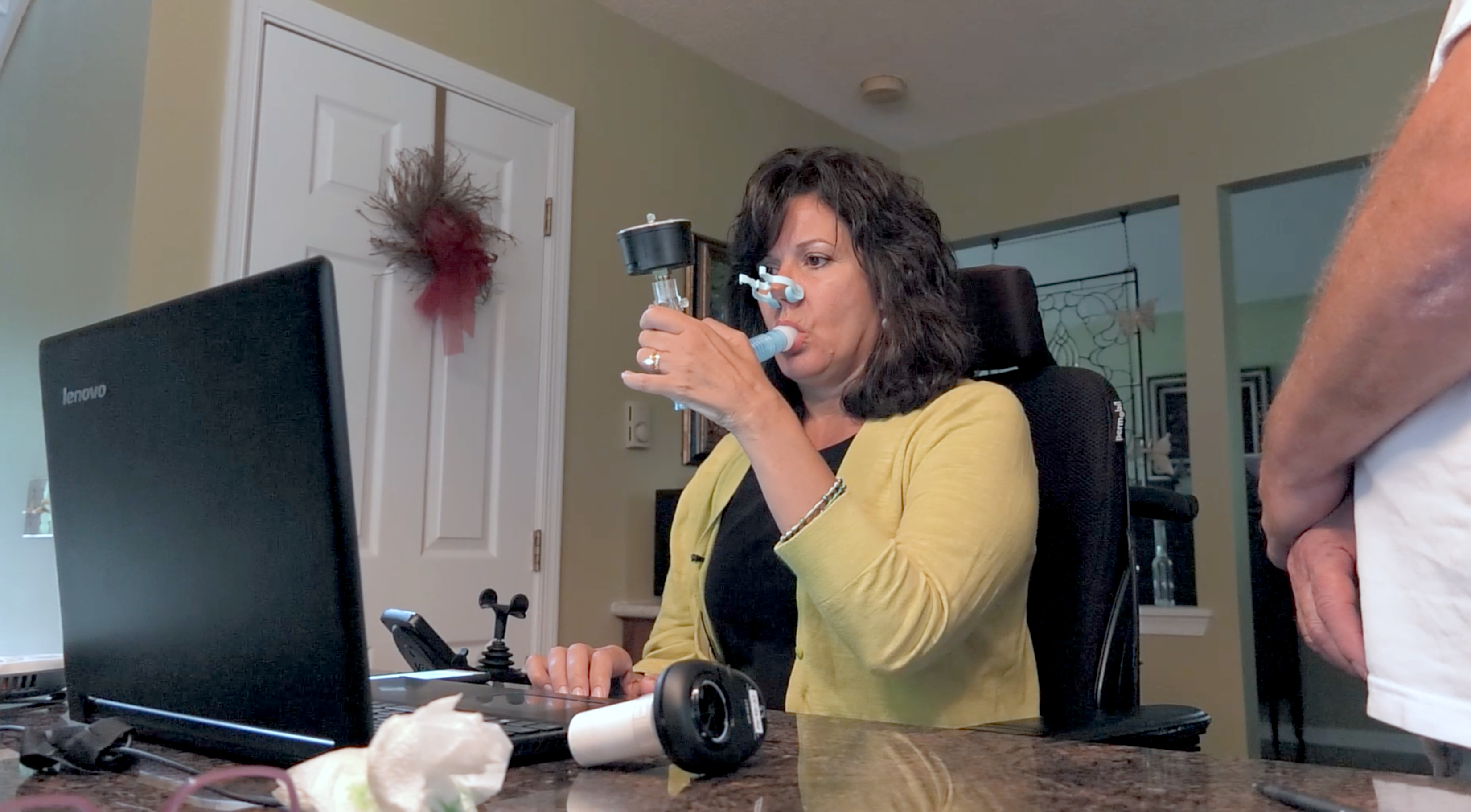
For Cynthia Lacey, the time, money and sheer energy it took to get to appointments in Hershey were an increasing challenge as her symptoms of ALS, or amyotrophic lateral sclerosis, a progressive neurodegenerative disease, progressed.
YouTube
MediaSite
The resident of Tobyhanna, Pa., located two hours northwest of Hershey, considers herself fortunate to be a patient at the Penn State Health Milton S. Hershey Medical Center ALS Clinic and Research Center, one of just three ALS treatment centers in the nation that offers virtual appointments to patients for whom travel is a challenge. For Lacey, it’s a 240-mile round trip.
“I used to dread the long trip so much that we came a day early and spent the money to stay overnight,” she said. “As a nurse myself, I am used to in-person assessments, but this works really well through a screen – and it saves us a lot of hassle.”
Now, sitting in the comfort of her living room, she says she has more energy for her three-hour appointments with Dr. Zachary Simmons, director of the Penn State ALS Clinic, and his clinical and research teams and finds her virtual care equal to in-person attention.
“The whole goal is to reduce the burden on a patient population for whom travel is difficult, endurance is reduced, and the trip makes for a gruelingly long day,” Simmons said. “A large part of the exam is making a visual assessment of what a patient can and can’t do. This format allows us to get the information we need, and we’ve had very positive feedback from patients.”
Penn State Health ALS OnDemand, which launched last October, is part of a growing telehealth program called Penn State Health OnDemand.
The overall OnDemand urgent care application, which launched to Penn State Health employees in August 2018, offers patients 24/7 urgent care service, said Christopher LaCoe, vice president of operations at Penn State Health Milton S. Hershey Medical Center, who oversees the entire telehealth program. It’s now available to anyone by logging in. There is no charge to enroll to have the app ready for use, no matter where the patient may be located. Patients who have no health insurance pay $49 cash for telehealth services. Those who do have insurance pay their standard co-pay for a visit.
“Digital care is the way of the future. Our goals are to reach more patients and save them time, money, effort, energy and open up accessibility to care from wherever they are and whenever it is convenient to them,” LaCoe said. “Enrollment is free, and once an individual is enrolled, the urgent care app offers the ability to log on, identify symptoms, select a provider of choice and receive care, all within about six to 10 minutes. Prescriptions can also be sent to the patient’s preferred pharmacy within that brief visit and be ready for pick-up shortly thereafter.”
Patients use secure video to connect face-to-face with a doctor. Up to four people can be connected, enabling family members in other locations to “attend” appointments if appropriate, for example, with older children who may be away at college or elderly family members who live separately.
“Sometimes the patient has to do the laying on of hands to better assess physical findings,” LaCoe said. For example, if strep throat is suspected, the patient can use a phone camera to take a picture of the throat to send to the doctor. Or a parent may tug on a child’s ear while the doctor observes whether the child winces, which may suggest an ear infection.
Since the urgent care app was launched, nearly 4,500 patients have downloaded it, and more than 600 visits have been conducted. Patient satisfaction with the service has been high, at 4.8 out of 5 stars for both providers and the technology, LaCoe said.
Bluetooth-enabled devices can integrate into the platform to track specific device readings for patients from wherever they are connecting. This is how Lacey documents her pulmonary function tests. Rather than checking results only every three months at on-site patient visits, these devices allow for continuous patient monitoring and lead to earlier intervention, Simmons said.
In the coming months, care for patients with inflammatory bowel disease, certain heart and vascular diagnoses and maternal-fetal medicine will be added to the offerings, LaCoe said. In the future, Penn State Health plans to add reproductive endocrinology and infertility care, behavioral health, specific surgical follow-up visits and lactation consultation. Penn State Health doctors see patients in the specialty OnDemand programs, he noted.
American Well, the organization that provides the OnDemand platform for all of the health system’s service lines, presented Penn State Health with the Clinical Delivery in the Digital Era award in June for its outstanding work utilizing American Well technology to drastically improve the care experience for ALS patients.
“We’re really gratified to see this program recognized,” Simmons said. “I’m very proud we’ve been able to do this here. It’s been very much a team effort between Penn State Health leadership and our ALS team.”
Simmons and his team of respiratory, occupational and physical therapists, nurses and other staff have done more than 75 ALS OnDemand visits so far, saving about 7,500 miles of travel for their patients.
For Lacey, who has lost the ability to walk and acknowledges that her breathing, speech and ability to swallow are slowly decreasing, Penn State Health OnDemand gives her one more tool to help her to handle her disease with grace.
“I pray an awful lot for strength, courage, guidance and hope as I get worse,” she said. “I get exhausted pretty frequently, and it helps to not have to leave home. I would recommend it to anyone.”
Research related to this project was funded through Penn State Clinical and Translational Science Institute’s Bridges to Translation III Pilot Grant Program.
To sign up for Penn State Health OnDemand, download the iOS or Android mobile app or visit PennStateHealthOnDemand.com.
If you're having trouble accessing this content, or would like it in another format, please email the Penn State College of Medicine web department.


