Penn State Health, Penn State College of Medicine experts share COVID-19 vaccine in Q&A
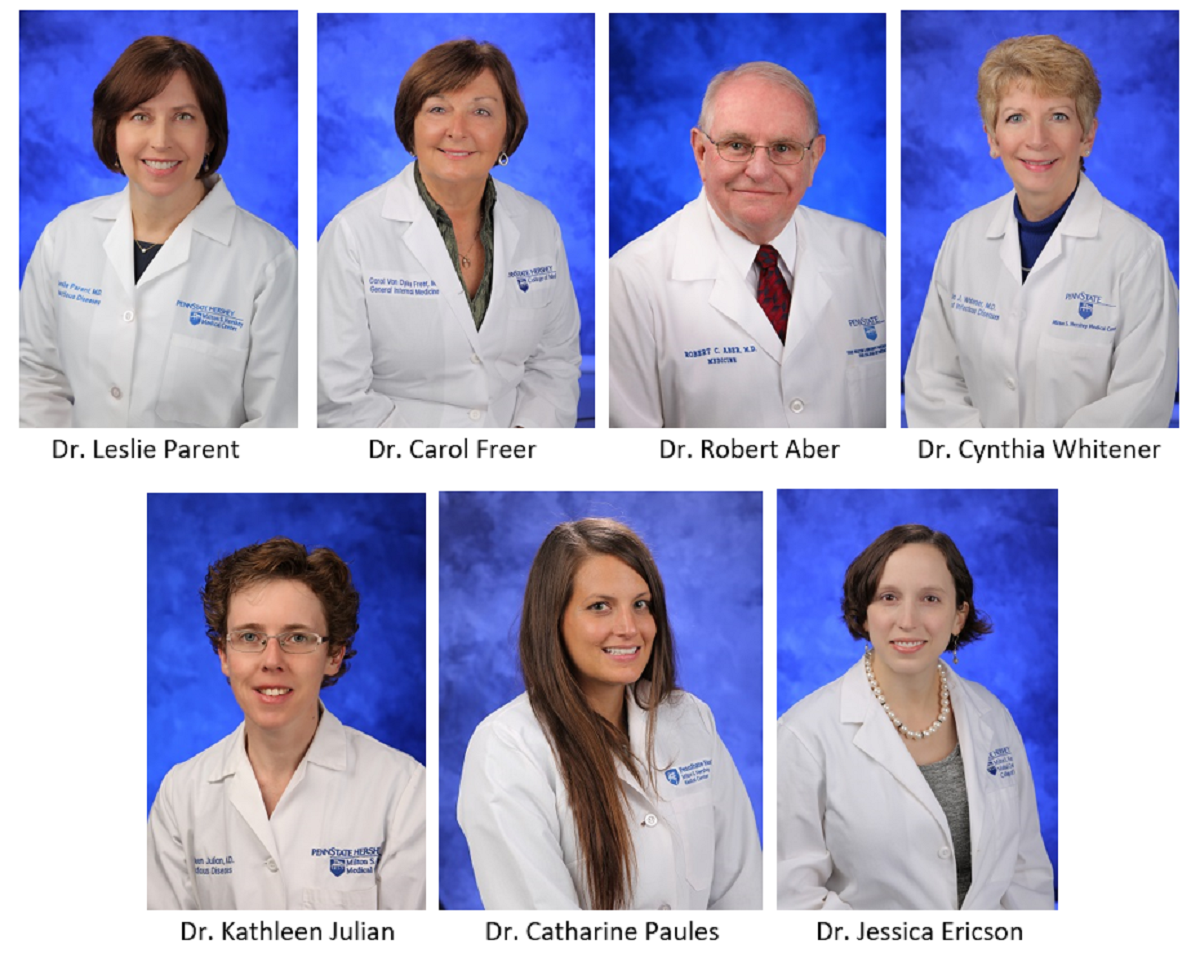
Seven Penn State Health and Penn State College of Medicine infectious disease experts have offered their colleagues answers to frequently asked questions about the vaccine.
Providing answers were Dr. Leslie Parent, vice dean for research and graduate studies; Dr. Carol Freer, infectious disease specialist/epidemiologist, Internal Medicine; Dr. Robert Aber, senior advisor to the dean; Dr. Cynthia Whitener, chief of the Division of Infectious Diseases at Hershey Medical Center; Dr. Kathleen Julian, infectious disease specialist; Dr. Catharine Paules, infectious disease specialist; and Dr. Jessica Ericson, assistant professor, Pediatrics and Infectious Diseases.
Below is their message for their colleagues at the College and health system:
As your colleagues who care for people with infectious diseases, we wanted to reach out to make sure anyone who is not yet vaccinated against COVID-19 has an opportunity to have their questions about the vaccines answered.
We understand that you may still be unsure about receiving a vaccination against COVID-19, and in a world where information is coming at you from multiple sources, we want to take a moment to provide some material that may be helpful to you as you consider this important decision.
Q: Was the vaccine developed so quickly that it may not be safe?
A: It’s important to know that all of the steps necessary to bring a vaccine to the public have been followed for the Food and Drug Administration (FDA) authorized and approved COVID-19 vaccines. You may not realize that these vaccines have undergone the most intensive safety monitoring in U.S. history. No regulatory steps were skipped.
These vaccines could be developed so quickly because scientists had a head start due to working on vaccines against SARS and MERS (two closely related coronaviruses). Scientists had also studied how to design platforms to make a new vaccine rapidly available. For example, mRNA vaccines have been studied over several decades against other viral infections, including Zika and influenza (flu). This type of vaccine introduces a small piece of mRNA into your cells which instructs your cell to make a viral protein. Your body then makes an immune response to this protein which protects you from serious illness. The mRNA is not incorporated into your DNA and is inactivated in a couple of days. The Moderna and Pfizer/BioNTech vaccines each utilize this technology. The Johnson & Johnson vaccine uses another type of platform, a viral vector, to generate a similar immune response.
The vaccines went through rigorous testing prior to receiving Emergency Use Authorization (EUA) from the FDA. The EUA allowed the vaccines to be disseminated rapidly to stem the pandemic while the FDA completed additional steps to fully approve the vaccines. While under EUA, rigorous safety monitoring was conducted and more than 166 million people in the U.S. have now been fully vaccinated according to the Centers for Disease Control and Prevention.
Significant side effects have been exceedingly rare. In pregnant women receiving the vaccine, no evidence exists for increased risk of miscarriage or harm to the fetus. Similarly, fertility is not affected by COVID-19 vaccination. On August 23, 2021 the Pfizer/BioNTech Vaccine was FDA approved. The Moderna vaccine is also being evaluated for full FDA approval.
Q: Will I feel sick after getting a COVID-19 vaccination?
A: You may develop side effects that are not serious but are uncomfortable. Many people develop a sore arm. Some people may have fever or headache, or they may feel achy and tired. We suggest that people plan their vaccination knowing that they may need extra rest the following day. These post-vaccination symptoms can be treated with over-the-counter medications like acetaminophen (Tylenol) or anti-inflammatory medications including ibuprofen (Advil or Motrin) or naproxen (Aleve), and typically resolve within a day or two. The thing to remember is these side effects are all signs that your immune system is working as it should. Even though it can be uncomfortable, be reassured that these reactions are temporary.
Q: If the vaccine is so effective, then why are vaccinated people still getting COVID-19?
A: No vaccine is 100% effective at preventing infection. Like other vaccines, breakthrough infections can occur, and most infections will be asymptomatic or mild. The most important factor for you to consider is that with the vaccine, the risk of hospitalization or death from the virus is dramatically reduced. This is because when you are vaccinated, your body mounts an immune response against the virus that causes COVID-19 that helps protect you from serious disease even if you do become infected. The vaccine is your best defense to prevent death or serious illness.
Q: What is the delta variant and can the vaccine protect me against it?
A: The virus that causes COVID-19 can mutate and change over time, picking up advantages over prior virus strains. This is what led to the emergence of the delta variant, which is spread more easily from person to person, may cause more severe illness, and causes more vaccine breakthroughs than prior strains. New variants will continue to arise throughout the world, and some may be more dangerous than the delta variant. By vaccinating as many people as possible, we can reduce the number who get infected, and there will be less virus replication and fewer mutants. The Moderna, Pfizer/BioNTech and Johnson & Johnson vaccines have been proven to be effective in reducing the chance of severe illness and hospitalization as a result of getting COVID-19 caused by the Delta variant.
Q: If I had COVID already, why do I need to get vaccinated?
A: It is important to realize that if you had COVID-19, you can get infected again. Recently a study found that people in Kentucky who had COVID-19 and were vaccinated had twofold better protection against re-infection that those who were previously infected but were not vaccinated. The vaccine makes a stronger immune response against the virus compared with natural infection, and scientists are still working to fully understand the reason for this. Even if you’ve had COVID-19, we would recommend getting the vaccine to ensure that you have a higher level of protective immunity.
Q: How do the Centers for Disease Control and Prevention and FDA monitor the long-term effects of COVID-19 vaccination?
A: There are several safety monitoring systems in place to track vaccine safety and identify possible problems. These systems include the V-safe app for self-reporting, the Vaccine Adverse Event Reporting System (VAERS), which allows anyone to submit a report of an adverse reaction to a vaccine, and the Vaccine Safety Datalink, which monitors large Health Maintenance Organizations across the country for possible adverse reactions. Even after more than 166 million people have been vaccinated, severe side effects have remained extremely rare. It’s important to realize that the vast majority of adverse effects occur in the first six weeks after receiving a vaccine. Information about the safety monitoring systems for COVID-19 vaccines are available here: https://www.fda.gov/vaccines-blood-biologics/safety.
Q: Will everyone need booster shots in the future?
A: An important remaining uncertainty is the duration of the immune response the vaccines generate against the virus that causes COVID-19. Recent information with the delta variant indicates that strong immunity may last for about 8 months and may then decrease over time. This is why the CDC and FDA are likely to soon give the green light to providing booster shots for those who are already vaccinated—to ramp up the protection against Delta variant and variants that may arise in the future.
Q: Do I need to continue to wear a mask after getting the COVID-19 vaccine?
A: It is very important to continue to wear a mask, practice physical distancing, avoid large gatherings, and wash your hands frequently even after getting the COVID-19 vaccine. Although you are likely protected from serious complications of COVID-19, it is possible to spread the virus to others, especially with the highly infectious delta variant, the most common virus subtype in the U.S.
With the rise of delta and other variants, we hope you will decide to be vaccinated soon. We do not want to see you or your family become seriously ill, end up in the hospital or die of COVID-19. COVID-19 can also cause long-term effects on the heart, brain, lungs and other systems that might make you feel unwell for quite a long time, and the vaccines can protect you against those long-term effects.
We hope this information was helpful to you. We recognize that the information about COVID-19 and vaccines has been changing rapidly, and it is hard to know what information you should trust. If you have any further questions or concerns, we encourage you to reach out to us at askacovidq@pennstatehealth.psu.edu or speak with your physician.
If you're having trouble accessing this content, or would like it in another format, please email the Penn State College of Medicine web department.
